 It’s a cliché that men never stop and ask for help when they’re lost. Unfortunately, the same is often true about men and health. Guys often put off getting help when they’re sick and pass it off as “no big deal”. Over 55% of men haven’t even had a physical in over a year according to a survey by The American Academy of Family Physicians. And recommended cancer screenings have decreased during the COVID-19 pandemic.
It’s a cliché that men never stop and ask for help when they’re lost. Unfortunately, the same is often true about men and health. Guys often put off getting help when they’re sick and pass it off as “no big deal”. Over 55% of men haven’t even had a physical in over a year according to a survey by The American Academy of Family Physicians. And recommended cancer screenings have decreased during the COVID-19 pandemic.
Procrastination can be dangerous, especially with cancer. Early screenings are essential for survival.
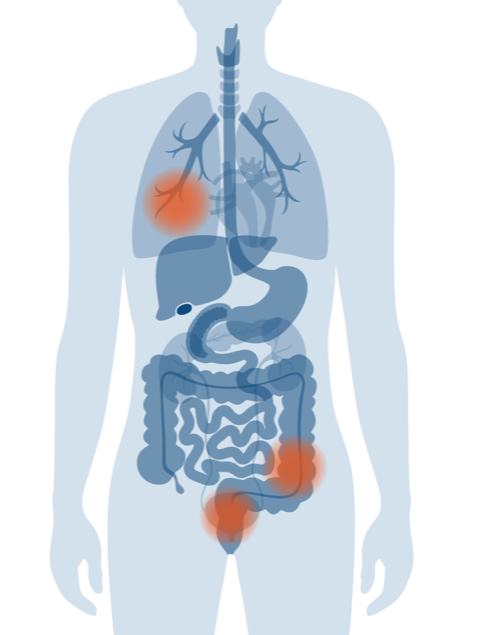
Beware of the Big Three: prostate, colorectal, and lung cancers
This trio is most common among men, and among the deadliest. Colorectal and lung cancer are actually equal-opportunity diseases – affecting men and women. But incidence rates are higher among men due to lifestyle factors.
Prostate cancer
Prostate cancer is the second most common cancer in men, behind skin cancer. But it’s a leading killer. This form of cancer is rare in younger men, but risk increases with age; about 60% of cases are men over 65.
 Prostate cancer can be insidious; some men don’t have any symptoms until it reaches an advanced stage. Dr. Somu Suppiah, Radiation Oncologist at Minneapolis Radiation Oncology says, “At MRO, we recommend prostate cancer screening – a digital exam or PSA blood test with your yearly physical – by age 40.”
Prostate cancer can be insidious; some men don’t have any symptoms until it reaches an advanced stage. Dr. Somu Suppiah, Radiation Oncologist at Minneapolis Radiation Oncology says, “At MRO, we recommend prostate cancer screening – a digital exam or PSA blood test with your yearly physical – by age 40.”
The good news is, with early detection, prostate cancer is very treatable. The American Cancer Society reports the 5-year survival rate for Stage 1 prostate cancer is nearly 100%, with long-term prospects over 90%.
Ethnic heritage plays a role in determining your risk. Prostate cancer is more common in African-American men, and less common in Asian-American and Latino men. Genetics also play a part; a father or brother with prostate cancer more than doubles your risk.
Different people have different symptoms. Once again, this underlines the importance of screening. But if you have any of these early signs, see your doctor right away.
- Difficulty starting urination.
- Weak or interrupted flow of urine.
- Frequent urination, especially at night.
- Difficulty emptying the bladder completely.
- Pain or burning during urination.
- Blood in the urine or semen.
- Pain in the back, hips, or pelvis that doesn’t go away.
- Painful ejaculation.
Lung Cancer
This is the biggest killer in men, accounting for over 1200 deaths a year in Minnesota men. Lung cancer is more common in men because men have higher rates of smoking. Men may also face higher exposure to carcinogenics in the workplace.
But smoking is linked to nearly 90% of lung cancer deaths. The CDC reports cigarette smokers are 15 to 30 times more likely to get lung cancer or die from it than non-smokers. Even secondhand smoke from other people’s cigarettes, pipes, or cigars causes lung cancer.
According to the EPA, naturally-occurring radon gas is the second leading cause of lung cancer. In Minnesota, it’s a serious public health risk: 40% of our homes have radon levels that pose a significant health risk. That’s more than three times higher than the U.S. average, because of our geology and because our homes are closed up or heated much of the year.
The American Cancer Society recommends a low-dose computed tomography scan (LDCT). once a year if you’re 55 to 80 years old, if you smoke now, have quit within the past 15 years, or if you smoked over a pack a day for 30 years.
Common early warnings of lung cancer are:
- A cough that does not go away or gets worse
- Coughing up blood or rust-colored sputum
- Chest pain that gets worse with deep breathing, coughing, or laughing
- Hoarseness
- Loss of appetite
- Unexplained weight loss
- Shortness of breath
- Feeling tired or weak
- Infections such as bronchitis and pneumonia that persist or recur
- Wheezing
Colorectal cancer
Nearly one-fifth of men ages 55 and over have never been screened for colorectal cancer. You should get screened between ages 50 and 75 – earlier if there’s a family history, or you’re at increased risk. That includes African-Americans, who have the highest colorectal cancer incidence and mortality of all racial groups in the US, and Jewish men of Eastern European descent.
Risk of colorectal cancer increases with age, especially after 50. Other risk factors include:
- Inflammatory bowel disease (Crohn’s disease or ulcerative colitis)
- Personal or family history of colorectal cancer or colorectal polyps.
- Sedentary lifestyle.
- A diet low in fruit and vegetables
- A low-fiber, high-fat diet, or a diet high in processed meats
- Obesity
- Increased alcohol consumption
- Tobacco use
The U.S. Preventive Services Task Force (USPSTF) recommends:
- Colonoscopy once every 10 years, or
- Sigmoidoscopy every 5 years, plus fecal occult blood test (FOBT) every 3 years
If your bowel movement schedule changes drastically over a few days, talk to your doctor. Blood in your stool is not a good sign, either. And the more common symptoms of colorectal cancer – diarrhea and constipation– often come together.
For more information on colorectal cancer, visit: https://mropa.com./community/get-tested-and-lower-your-risk-of-colorectal-cancer/
Be a stand-up guy and stand up against cancer.
There’s no sure-fire prevention for cancer. But there are habits you can change to cut your risk, and increase your chances for a longer, healthier life. It’s not rocket science, just common sense.
- Watch what you eat. Ease back on red meat and processed meats. Eat your vegetables.
- Get off the couch. Twenty minutes of moderate exercise a day can work wonders for your overall health.
- Quit smoking. It’s one of the best things you can do for your health overall.
- Lay off the booze. Enjoy your favorite beverage, but in moderation.
- See your doctor once a year. Get a physical and get regular screenings.