What is Radiation Therapy
Radiation therapy, sometimes called radiotherapy, involves the use of high-energy X-rays, to treat cancer and other diseases. Radiation has been used to effectively fight cancer for over 100 years. At Minneapolis Radiation Oncology (MRO), radiation oncologists use radiation to cure cancer, to shrink or stop a tumor from growing, or to relieve pain.
Radiation is a localized treatment, that only targets the cells in the part of the body being treated. It’s often used along with other cancer treatments, such as surgery, chemotherapy, or immunotherapy.
How does radiation therapy work?
At MRO, the doctor and care team direct radiation beams to the tumor inside your body to destroy or damage cancer cells, so they can no longer reproduce; this slows or stops tumor growth. Radiation therapy can be administered externally or internally based on the recommended treatment plan created for you, dependent on your cancer type, location, and stage. Your doctor will discuss your treatment options and answer your questions in depth before you begin any treatment.
Most cancer patients have external beam radiation therapy delivered from a state-of-the-art machine called a linear accelerator (LINAC). With the continued introduction of advanced imaging and sculpting tools we can use the LINAC to precisely target a tumor with three-dimensional accuracy that shapes and directs the beams with precision. This results in the ability to treat with fewer potential side effects.
MRO has been awarded full accreditation in excellence of care and safety by the American Society of Radiation Oncology APEx program.
What are the benefits and risks of radiation therapy?
Benefits
Radiation is an effective way to treat many different types of cancer, in almost any part of the body. At least half of all people who are treated for cancer receive radiation therapy and the number of patients cured rises every day.
Even when a cure is not possible, radiation therapy may bring relief. Many patients can enjoy a better quality of life when radiation is used to shrink tumors and reduce pressure, bleeding, pain, or other symptoms.
Risks
Like many other treatments for disease, there are risks involved with radiation therapy. The brief doses of radiation that destroy cancer cells can also damage normal cells. When this happens, you may experience side effects, but generally, the risk of side effects is outweighed by the benefits of killing cancer cells. Your MRO care team will not recommend radiation treatment unless the potential benefits are greater than the known risks.
Every person reacts to radiation therapy differently. It’s best to consider that side effects are possible, though you may not experience any of them. Your MRO care team can help you determine how to prevent or manage side effects.
Treating your cancer with radiation therapy

A cancer diagnosis is life changing. As specialists in treating cancer with advanced radiation technology, we understand that the more you know about your treatment options, the better you can make informed decisions and get back to living your life.
The care teams at MRO provide the highest standards of care, using the most advanced radiation technology available. We provide multiple modalities of therapy: external and internal treatments for cancer, as well as therapies for other noncancerous conditions.
External beam radiation therapy (Conventional)
External beam radiation therapy (Conventional) is the most common method for delivering radiation therapy. Typically, external beam radiation uses small dosages of radiation, given 5 days a week over 1 to 8 weeks with breaks on the weekends. Patients who receive external radiation treatment are not radioactive during or after treatment.
External beam radiation therapy is delivered from a machine called a linear accelerator (LINAC). In the 1950’s, the LINAC revolutionized the way radiation was delivered to treat cancer. Now, we can use the LINAC to precisely target, sculpt, and conform radiation beams with these state-of-the-art tools:
-
MLC
Multi-Leaf Collimators (MLC) use leaves to automatically sculpt radiation beams to conform to the shape of a tumor from several different angles, allowing us to deliver a prescribed dose across all the dimensions of the tumor.
-
IMRT
Intensity-modulated radiation therapy (IMRT) is an advanced form of three-dimensional radiation therapy. It allows our MRO care team to aim precisely shaped beams from the linear accelerator at the tumor from several directions and adjust the intensity of the beams.
IMRT radiation may also be delivered with a continuous arc of radiation that is constantly being shaped to conform to the target and your anatomy. This is often called RapidArc or VMAT (Volumetric Arc Therapy). Another advantage of arc-based technology is that your treatment time is much shorter.
-
IGRT
Image-guided radiation therapy (IGRT) involves daily imaging immediately before and/or during a treatment to verify the precise positioning of the target and radiation beams. Because tumors can move slightly from day to day, or even moment to moment during a treatment (such as a lung treatment when you breathe), we use IGRT to make precise adjustments. This enables us to optimize your daily treatment and minimize the dose to nearby normal tissues.
In addition to IGRT, MRO therapy centers are equipped with other techniques to ensure precise localization. For example, in certain cases, we can directly monitor the external contour of a patient’s body, to ensure precise positioning and account for motion during breathing. These techniques are important during breast cancer treatment, helping to not expose the heart to radiation.
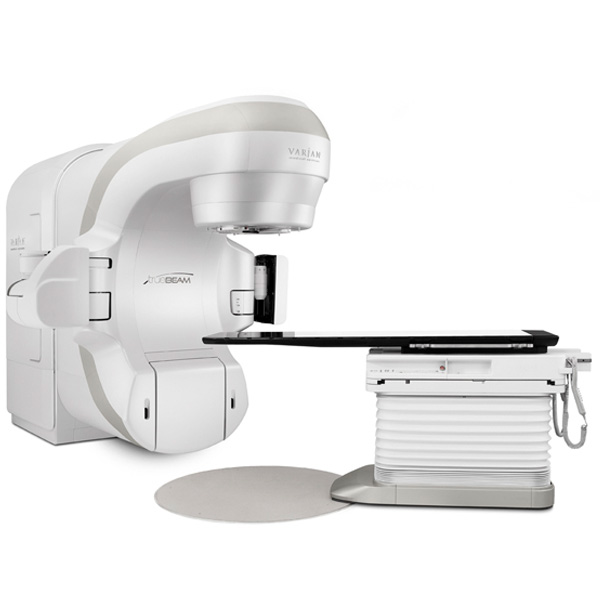
LINAC Machine

RapidArc

MLC
Stereotactic Radiotherapy
Stereotactic Radiotherapy is a specialized type of external beam radiation therapy that uses highly focused megavoltage x-ray beams to shrink or control the growth of a tumor or abnormal cells by either killing the cells directly, or by disrupting the ability of the cells to grow. Stereotactic radiation therapy is a highly conformal treatment that delivers a very high dose of radiation in only a few treatments. The treatment(s) are delivered in 1-5 fractions over the course of 1-2 weeks.
For stereotactic radiation therapy, it is extremely important to use an immobilizing system that will allow patients to be accurately repositioned to match their position on the day of CT-based planning.
Your MRO care team may use stereotactic radiotherapy because of a tumor’s location, because of a high risk of side effects with other treatments, because a patient is not healthy enough for other treatments, or
because a tumor continues to grow despite other treatment. Your MRO care team can tell you if this is an option for your specific condition.

There are two types of stereotactic radiation:
- Stereotactic body radiation therapy (SBRT), sometimes called stereotactic ablative radiotherapy (SABR), delivers precisely focused – down to the millimeter – radiation in typically three to five treatments to tumors within the body.
- Stereotactic radiosurgery (SRS) typically delivers one stereotactic radiation treatment to the brain. SRS is delivered by a team involving a radiation oncologist and neurosurgeon. This treatment does not involve surgery. An incision is not made, and tissue is not surgically removed. You’ll be fitted with a mask system worn during preparation and treatments to keep your head in the same precise position.
Stereotactic Radiation (SRS/SBRT/SABR) is generally best for very small tumors. The doctors at MRO use specialized scans to pinpoint the exact tumor location and adjust for patient motion, such as breathing. A customized holder or mask may be used to keep the body perfectly still during treatment. Some patients with more than one target area could have treatments using a combination of SRS, SBRT/SABR, and conventional radiation therapy.

HyperArc is an automated treatment delivery paradigm, which aims radiation at tumors from a variety of beam angles. HyperArc allows the specialists at MRO to irradiate multiple brain tumors at the same time without the need to reposition the patient. This new technology is designed to help treat patients with multiple brain metastases significantly faster and more efficiently.
Internal Radiation Therapy—Brachytherapy
Internal radiation, or brachytherapy may be recommended for certain types of cancer, such as prostate cancer or cervical cancer. In fact, MRO pioneered this type of treatment for prostate cancer in 1988.
 With brachytherapy, a radioactive implant is put inside the body in or near the tumor. This way the radiation affects as few normal cells as possible. Getting the implant placed is usually done in a hospital. Depending on your type of cancer and treatment plan, you might get a temporary or a permanent implant.
With brachytherapy, a radioactive implant is put inside the body in or near the tumor. This way the radiation affects as few normal cells as possible. Getting the implant placed is usually done in a hospital. Depending on your type of cancer and treatment plan, you might get a temporary or a permanent implant.
- Low-dose-rate brachytherapy (LDR) which is often administered for prostate cancer – uses an implant that gives off lower doses of radiation over a longer period. Implants may be left in place for a day or so, but some smaller implants are left in place and never taken out. They’re about the size of a grain of rice and rarely cause problems and after several weeks, they stop giving off radiation. If your implants are to be left in, you may be able to go home the same day they’re put in. Your body may give off a small amount of radiation for a short time, and your MRO care team may recommend you take some special precautions after treatment.
Prostate Brachytherapy
Minneapolis Radiation Oncology physicians pioneered the use of brachytherapy for prostate cancer in the upper Midwest. The first treatment in the region was performed by MRO radiation oncologist Dr. Doug Olson in 1988. Prostate brachytherapy is performed in a specially equipped operating room by a radiation oncologist and a urologist while a patient is asleep or under anesthesia. Working closely together the team uses ultrasound guidance to place long thin metal tubes into the prostate, through which 70 to 120 tiny radioactive seeds are implanted. The seeds are about the thickness of a pencil lead and just about an 1/8 inch long. The procedure typically takes one hour, and the patient is usually discharged later that day. Although the internal seeds emit low-energy radiation with only trace amounts of radiation outside the patient’s body, the specialists at MRO recommend patients avoid close contact with children and pregnant women for a short time following the seed placement. After approximately 6 months, the seed will be essentially inactive. They can be safely left in place indefinitely. - High-dose-rate brachytherapy (HDR) treats patients for several minutes at a time with a powerful radioactive source that’s put in an applicator. The source is removed after 10 to 20 minutes. You may be treated twice a day over a few days, or once a day over the course of a few weeks. The radioactive material itself is not left in your body, but the applicator might be left in place between treatments, or it might be put in before each treatment. The radioactive source is removed from your body after HDR brachytherapy, and you are not radioactive after treatment.